Nutrition for the ageing bone
14 important questions on Nutrition for the ageing bone
What is the difinition of osteoporosis?
"A progressive systemic skeletal disease characterized by low bone mass and micro architectural deterioration of bone tissue, with consequent increase in bone fragility and susceptibility of fracture
What is the process of bone turnover?
- Osteoclasts break down bone creating a resorption cavity
Formation
- Osteoblasts make new bone matric which is then mineralised, filling the remodelling space
Enable bone to
- adapt to mechanical loading
- repair damage
- regulate circulating Ca levels
- contribute to acid/base balance
What are the markers of bone turnover?
- regulators of bone turnover
- bone formation markers
- bone resorption markers
- PYD / DPD
- Higher grades + faster learning
- Never study anything twice
- 100% sure, 100% understanding
What are the changes in bone mass with ageing
- Attainment of peak bone mass
- Consolidation
- Age related bone loss
What are the influences of calcium on bone health? And what are the requirements
- PTH (parathyroid hormone)
- stimulates Ca2+ uptake in kidneys
- active vitamin D
- increases Ca2+ uptake in intestines
- stimulates Ca2+ release from bones
- blood Ca2+ level rises
- homeostasis: blood Ca2+ level (about 10 mg/100ml)
- Stimulus: falling blood Ca2+ level
The calcium requirements are 700mg for 19-50 and 51-70
Lower reference nutrient intake (LRNI) is 400mg/d
What are the influences of calcium on bone health? And what are the requirements
- PTH (parathyroid hormone)
- stimulates Ca2+ uptake in kidneys
- active vitamin D
- increases Ca2+ uptake in intestines
- stimulates Ca2+ release from bones
- blood Ca2+ level rises
- homeostasis: blood Ca2+ level (about 10 mg/100ml)
- Stimulus: falling blood Ca2+ level
The calcium requirements are 700mg for 19-50 and 51-70
Lower reference nutrient intake (LRNI) is 400mg/d
What is the mechanism behind the acid-base homeostasis
- (diet)When the human body is confronted with an excess of H2 ions from the diet, it employs a number of strategies to maintain normal blood (pH (7.4)
- (lung)pulmonary regulation of the biocarbonate - carbonic acid buffer system (respiratory compensation)
- (kidney)elimination of non volatile acids or Na HCO3
What is the mechanism of action for the acid-base homeostasis?
- Direct enhancement of osteoclastic activity - cell mediated vs. Simple passive physicochemical exchange?
- tiny changes in extracellular pH close to physiological range - results in large (but independent) alterations in osteoclastic & osteoblastic activity
- direct enhancement of osteoclastic activity H+ ions
- low plasma pH - enhanced Ca release - indirectly via PTH
- 'in vitro' method of assessing bone resorption by disaggregated osteoclasts
- lowering medium pH - enhanced osteoclastic activity - independent of PTH
What is the evidence of acid-base/fruit & vegetable effect in the DASH study
- Increasing fruit & vegetable intake from 3.6 to 9.5 daily servings
- urinary Ca 157mg/d to 110 mg/d - change of 47mg/d
- urinary Ca of controls decreased by only 14 mg/d
discussion
- unexpected observations were a prominent reduction in urinary Ca excretion .... Explained by the high fibre content of these two diets, which may have impeded Ca absorption
- an alternative theory 'reduction in acid load of the diet in those subjects on the high fruit & vegetable component'
DASH-sodium diet bone resorption marker: decrease CTx: 16-18%
What is the evidence of acid-base/fruit & vegetable effect in the DASH study
- Increasing fruit & vegetable intake from 3.6 to 9.5 daily servings
- urinary Ca 157mg/d to 110 mg/d - change of 47mg/d
- urinary Ca of controls decreased by only 14 mg/d
discussion
- unexpected observations were a prominent reduction in urinary Ca excretion .... Explained by the high fibre content of these two diets, which may have impeded Ca absorption
- an alternative theory 'reduction in acid load of the diet in those subjects on the high fruit & vegetable component'
DASH-sodium diet bone resorption marker: decrease CTx: 16-18%
What is vitamin D?
- the term 'vitamin D' is a confusing; it is not a 'vital amine' in the true sense of the word. It is a pro-hormone
Only nutrient where main source is not diet but UV exposure
- UVB exposure must be at 290-315nm
- vitamin D is absolutely critical to health
- children rickets
- adults osteomalacia; osteoporosis
- heart disease
- diabetes
- cancer
- TB
- the common cold
- (in the UK, we can only make vitamin D between April to September; British winter is a huge challenge for vitamin D health!)
Vitamin D metabolism
What are the vitamin D recommendations
- defining vitamin D deficiency adequacy
- uk recommendations
- Scientific advisory committee on Nutrition (UK)
- institute of medicine (north America)
- European food safety authority
- endocrien society
- 10 mug/day
Aim: does it matter if you give vitamin D2 (plant source) or vitamin D3 (animal sources)? What is the outcome?
impact: key information for DoH, PHE and the food industry...; led to exciting bid for further significant funding from BBSRC DRING II
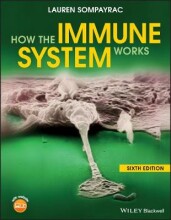
The question on the page originate from the summary of the following study material:
- A unique study and practice tool
- Never study anything twice again
- Get the grades you hope for
- 100% sure, 100% understanding